Urbanization has increased the incidence of respiratory tract infections.
Asthma (also termed "bronchial asthma") is an inflammatory condition of the smooth muscles lining the airways. It is a chronic condition affecting all age groups, especially children and young adults.
Nearly 300 million people worldwide are suffering from asthma, out of which 6% of the cases are seen in children while 2% contribute to adult asthma. The prevalence of asthma increases by 50% every passing decade. Nearly 2/3rd of asthma cases are diagnosed before the age of 18 years. In India, nearly 30 million people are asthmatic. Every year about 4.5 lakh people die from asthma worldwide, with a mortality rate of 2 lakh in India.
Pathophysiology of asthma
Asthma is mainly characterized by varying degrees of airflow obstruction (related to swelling, bronchospasm and hypersecretion) and airway inflammation. In asthma, all the cells of the airways are involved and get activated, such as epithelial cells, eosinophils, T cells, mast cells, macrophages, fibroblasts and bronchial smooth muscle cells.
The inflammatory reaction can be divided into two phases: early and late-phase.
On exposure to allergens, the body releases and activates various cells containing allergen-specific IgE (antibodies specific to allergens), such as mast cells and macrophages. These cells release pro-inflammatory mediators (chemicals) like histamine, eicosanoids and reactive oxygen species that cause airway smooth muscle contraction, mucus secretion and dilatation of the blood vessels. This is termed the early-phase inflammatory reaction.
The late-phase inflammatory reaction occurs after a few hours (about 6-9 hours) of allergen exposure. In this phase, the body activates other inflammatory cells such as eosinophils, CD4+ T cells, basophils, neutrophils, and macrophages.
Classification of asthma
Asthma can be classified into various types
1. Based on the severity
Intermittent: The symptoms are mild and don't interfere with sleep and regular activities. The symptoms will occur less than twice a week. On examination, the lung function is normal. The chances of an asthma attack are very less.
Persistent
- Mild: The symptoms may occur more than twice a week but not daily. It may slightly interfere with sleep (3-4 times a month) and regular activities. On examination, the lung function is normal. An asthma attack can occur more than twice a year (in children, it can be more than twice in six months or four or more episodes of wheezing in a year that lasts for more than one day).
- Moderate: In moderate persistent asthma, the symptoms occur daily with nighttime waking up to 3-4 times a month (or more than once a week). It may cause some limitations in regular activities. On examination, there may be a slight reduction in lung function (up to a 5% reduction). The occurrence of asthma attacks is similar to that seen in mild persistent asthma.
- Severe: In severe persistent asthma, the symptoms of asthma occur throughout the day, with nighttime waking seen often every day. Regular activities are extremely limited, and on examination, the lung function is reduced by more than 5%. Similar to mild persistent asthma, asthma attacks can occur more than twice a year.
2. Based on triggering factors
Allergic asthma: Asthma can be triggered by various allergens such as pollen, dust, animal fur, some chemicals, paints, certain medicines, cold air, some foods, etc.
- Temporary asthma: Some people may or may not have asthma, but when exposed to specific allergens, they show asthma-like symptoms.
- Seasonal: In some people, the asthma symptoms flare up only during a particular season, especially during the rainy and winter seasons (when there are increased number of pollen and during cold). People with seasonal asthma may also have other related conditions like hay fever (seasonal allergies).
- Occupational: people who work at chemical factories, bakeries, agricultural fields, spice and food factories, printing presses, plastic, rubber and wood factories and other places where there is a lot of smoke and dust are prone to develop asthma. These people show asthma flare-ups when exposed to such occupational allergens.
Non-allergic asthma
- Exercise-induced asthma (bronchospasm): Some people may not have asthma but may show asthma-like symptoms, such as wheezing and breathlessness only after exercise. It is common in a dry and cold climate.
- Medicines: Some medicine such as aspirin and other NSAIDs (Non-steroidal anti-inflammatory drugs), benzalkonium chloride (preservative), and beta-blockers (eg: propranolol, labetalol, carvedilol, etc.)
- Respiratory tract infections: The common respiratory tract infections such as common cold, pharyngitis, sinusitis, and bronchitis may contribute to asthma-like symptoms or may even trigger the symptoms of asthma.
3. Based on age
Adult onset asthma: It is also termed "late-onset asthma". Generally, people develop asthma in early childhood, but some people may show asthma symptoms in adulthood (above 18 years of age).
- Occupational: As discussed above, occupational asthma occurs due to exposure to allergens based on occupation.
- Smoking
- Stress
Childhood asthma: Asthma can affect any age group of individuals. But it is most common in children below 5 years of age.
4. Based on gender
Hormones: The female hormones are more likely to be associated with asthma, which makes women more prone to asthma than men.
Asthma can also be classified as
- Acute asthma
- Chronic asthma
- Acute severe asthma
In this type of asthma, an asthma episode may progress for several days or hours, or the progression is seen rapidly over 1 to 2 hours. The patient may hardly say a few words with each breath and is generally poorly responsive or unresponsive to the usual medicines (i.e., bronchodilators).
- Exercise-induced bronchospasm
Some people may not be diagnosed with asthma but may show asthma-like symptoms only during vigorous exercise. People with persistent asthma may often experience exercise-induced bronchospasm (EIB). People mainly experience EIB during cold and dry weather.
- Nocturnal asthma
The worsening of asthma symptoms during the nighttime is termed "nocturnal asthma". It is most common in people with persistent asthma. Various factors may contribute to nocturnal asthma such as allergies, environmental changes at night (cold weather), GERD (reflux of gastric acid contents into the oesophagus may cause constriction of the airways), obstructive sleep apnea, sinusitis, and other respiratory tract infections.
- Asthma-COPD overlap syndrome (ACOS)
Some people may have both asthma and COPD. People with asthma who smoke are more prone to get ACOS. People with ACOS experience symptoms with a greater frequency and severity than either condition alone.
Another way to classify asthma is:
It is also termed "allergic asthma". It is caused by an allergic reaction provoked by allergens such as pollen, dust, some food, etc. A blood test shows an increased level of IgE antibodies (antibodies specific to allergens)
Intrinsic asthma
Intrinsic asthma is triggered by non-allergens such as cold and dry air, smoke, respiratory tract infection, stress, emotional status (anxiety, laughter, or crying may provoke asthma) and more.
How BIBO helps!
Asthma may not be cured irrespective of its type, but proper management can help improve the quality of life. It is always better to consult a doctor regularly instead of waiting for the symptoms to get worse. Following the right diet and lifestyle changes along with the medicines prescribed will help to manage the symptoms better.
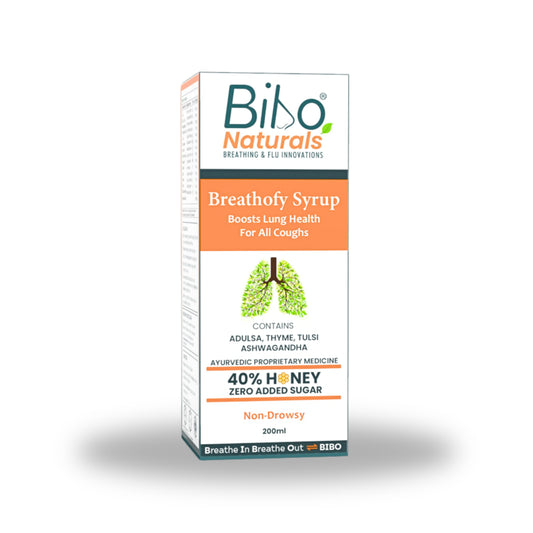
- Breathofy syrup: It is a lung supplement that helps to manage both acute and chronic respiratory conditions. The herbs like Tulsi, Mulethi, Adulsa, Rudravanti, Honey and a few more show anti-inflammatory and anti-asthmatic properties.
- Bibo Breathe Blend: It contains essential oils like Eucalyptus, Peppermint (menthol), Pine, Camphor and Thyme oil that helps to reduce the inflammation in the airways. Menthol is also proven to reduce dyspnea (which is a common symptom in asthma).
- Bibo clear vapor path ultra: The essential oils [Eucalyptus, Peppermint (menthol), Camphor and Thyme oil] of clear vapor patch ultra helps to open the nasal passages and airways for clear breathing. It also reduces dyspnea associated with asthma.
FAQs
Can you have asthma and not the symptoms for a long time?
Yes, intermittent asthma is a type of asthma which is generally mild, and people may not experience the symptoms for a year or more.
Can you have asthma and bronchitis simultaneously?
Asthma-COPD overlap syndrome is the presence of asthma and COPD (including bronchitis and emphysema) simultaneously. People with ACOS experience more frequent and severe symptoms than either condition alone.
Keywords: Asthma, Bronchial asthma, Pathophysiology of asthma, Types of asthma, Allergic asthma, Non-allergic asthma, Mild-moderate-severe asthma, GERD induced asthma, Extrinsic and intrinsic asthma, temporary asthma, asthma infection, Chronic bronchial asthma, Esophageal asthma.
References:
- National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2007 Aug. Section 2, Definition, Pathophysiology and Pathogenesis of Asthma, and Natural History of Asthma.
- Quirt, J., Hildebrand, K.J., Mazza, J. et al. Asthma. Allergy Asthma Clin Immunol 14, 50 (2018).
- Quirt J, Hildebrand KJ, Mazza J, Noya F, Kim H. Asthma. Allergy Asthma Clin Immunol. 2018 Sep 12;14(Suppl 2):50.
- Louie S, Zeki AA, Schivo M, Chan AL, Yoneda KY, Avdalovic M, Morrissey BM, Albertson TE. The asthma-chronic obstructive pulmonary disease overlap syndrome: pharmacotherapeutic considerations. Expert Rev Clin Pharmacol. 2013 Mar;6(2):197-219.